SHARE
Arthritis is a common condition that causes pain, swelling, and stiffness in the joints. There are over 100 types of arthritis, with the two most common being Rheumatoid Arthritis (RA) and Psoriatic Arthritis (PsA). Both Rheumatoid Arthritis (RA) and Psoriatic Arthritis (PsA) are autoimmune diseases that can look alike but there are also some key differences between the two.
In this article, we’ll compare rheumatoid arthritis vs. psoriatic arthritis and understand how they are related – covering the symptoms, causes, and treatment options for each.
Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune disease where the immune system mistakenly attacks the lining of the joints, known as the synovium. This causes swelling, pain and joint damage over time.
Key facts about Rheumatoid Arthritis:
- Affects around 1.3 million Americans. Women are up to 3 times more likely to develop Rheumatoid Arthritis than men.
- Often starts between ages 30-60, but can occur at any age.
- Causes swelling, pain and stiffness in joint areas like the hands, wrists, feet and knees.
- Has no known cure, but symptoms can be managed with medication.
- Can lead to permanent joint damage and disability if not treated.
- Has both genetic and environmental risk factors. Smoking is a major preventable risk factor.
Symptoms of Rheumatoid Arthritis
The most common symptoms of rheumatoid arthritis include:
- Joint Pain – Severe pain in the joints, especially in the smaller joints of the hands and feet.
- Joint Stiffness – Joints can feel stiff, particularly after periods of rest or inactivity.
In more severe Rheumatoid Arthritis, joint deformities can occur over time. Joint damage can lead to disability, especially when the condition goes unmanaged. That’s why early diagnosis and treatment are critical.
What Causes Rheumatoid Arthritis?
The exact causes of Rheumatoid Arthritis are not fully understood. However, it’s believed to be triggered by a combination of genetic and environmental factors:
Genetic Factors
- Inherited genes are a major contributor. Certain HLA genes appear to increase Rheumatoid Arthritis risk.
- Having a family history of Rheumatoid Arthritis raises your risk.
Environmental Factors
- Smoking – The biggest preventable risk factor. It may trigger Rheumatoid Arthritis in genetically susceptible people.
- Infections – Bacterial or viral infections could potentially trigger autoimmunity in some cases.
- Hormones – Rheumatoid Arthritis is more common in women. Hormonal factors may play a role.
- Obesity – Carrying excess fat may increase immune system activity, raising Rheumatoid Arthritis risk.
The immune system appears to malfunction, causing inflammation in the joints. What exactly triggers this is still being investigated.
Diagnosing Rheumatoid Arthritis
There is no single test to definitively diagnose rheumatoid arthritis. Doctors will use a combination of factors:
- Physical examination of joints for swelling, redness and warmth.
- Medical history, including pattern of joint symptoms.
- Blood tests to detect inflammation and antibodies like rheumatoid factor or anti-CCP.
- Imaging tests like ultrasound or MRI to assess joint damage.
Experiencing joint pain doesn’t necessarily mean you have Rheumatoid Arthritis. It’s important to see a rheumatologist (arthritis specialist) for an accurate diagnosis, especially if symptoms persist for over 6 weeks.
Treating Rheumatoid Arthritis
While there’s no Rheumatoid Arthritis cure, current treatments can effectively control symptoms and improve quality of life. The goals are to reduce inflammation, relieve pain, slow or prevent joint damage, and maintain function.
Common Rheumatoid Arthritis medications include:
- Anti-inflammatory drugs – Over-the-counter NSAIDs or prescription options.
- Steroids – Powerful anti-inflammatories like prednisone to quickly control flares.
- DMARDs – Disease-modifying antirheumatic drugs that slow progression.
- Biologics – Targeted therapies that block parts of the immune response.
- JAK inhibitors – Newer oral medications that inhibit inflammatory pathways.
- Pain medication – Opioids or NSAIDs for pain relief.
- Surgery – Only if joints are severely damaged.
The earlier that treatment begins, the better the outcome. A rheumatologist will tailor the medications to the patient’s specific case. Treating Rheumatoid Arthritis requires an ongoing approach to keep symptoms under control.
Psoriatic Arthritis
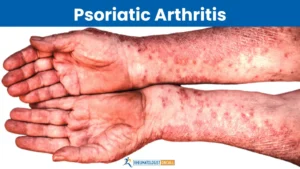
Like rheumatoid arthritis, Psoriatic Arthritis is an autoimmune inflammatory disease. But it only occurs in people who have psoriasis – an autoimmune skin condition.
Around 30% of psoriasis patients develop psoriatic arthritis. The typical onset is between ages 30-50, but it can develop at any age.
Quick facts about Psoriatic Arthritis:
- Occurs only in people with the skin condition psoriasis. Up to 30% of psoriasis patients develop it.
- Causes joint pain, swelling and damage. Can result in permanent deformities without treatment.
- Considered a seronegative spondyloarthropathy. Blood tests are often negative.
- Asymmetric arthritis that commonly affects the knees, fingers, toes, lower back and neck.
- No cure, but symptoms can be managed with medication and lifestyle changes.
- Requires collaboration between a rheumatologist and dermatologist.
Let’s go over the distinguishing symptoms of psoriatic arthritis, its causes, and risk factors.
Symptoms of Psoriatic Arthritis
The most common signs of Psoriatic Arthritis include:
- Joint pain – Stiffness and throbbing pain in the joints. The joints typically feel worse in the mornings.
- Swelling – Joints may become inflamed. Fingers and toes can appear sausage-like.
- Joint redness and warmth – The affected joints often feel warm to the touch.
- Limited range of motion – Joint stiffness can make movement difficult. Loss of function over time.
- Nail changes – Pitting, grooves or discoloration of the nails.
- Eye issues – Some people develop uveitis (eye inflammation).
Usually psoriatic arthritis develops about 10 years after the onset of psoriasis symptoms. However, in some cases it can precede skin symptoms.
What Causes Psoriatic Arthritis?
The exact underlying cause of Psoriatic Arthritis is unclear. However, it involves problems with the immune system and appears to have genetic factors:
- Immune dysfunction – Faulty immune signaling triggers inflammation in the joints and skin. Certain immune cells and inflammatory cytokines are overproduced.
- Genetic predisposition – Having certain genes makes someone more susceptible, especially in the presence of a trigger.
- Autoimmune response – The immune system mistakenly attacks healthy cells, including in the skin and joints.
- Trigger factors – Infections, physical trauma or stress can potentially set off psoriatic arthritis in those with a genetic predisposition.
Research continues on the interplay between genetics and environmental factors that contribute to psoriatic arthritis. There are likely multiple pathways that can lead to its development.
Risk Factors for Psoriatic Arthritis
Certain factors increase the likelihood of developing psoriatic arthritis:
- Psoriasis – Between 10-30% of psoriasis patients will get psoriatic arthritis.
- Family history – Having a close family member with it raises risk.
- Genetics – Variations in HLA genes seem to raise susceptibility.
- Age – Most commonly strikes between ages 30-50.
- Skin trauma – An injury can trigger a psoriasis flare-up.
- Strep throat infection – Can trigger guttate psoriasis in some people.
- Smoking – Might be a risk factor but the link is still being studied.
- Obesity – Excess weight may contribute to the inflammatory process.
The number one risk factor is being diagnosed with psoriasis, especially if you have a family history of psoriatic arthritis.
Diagnosing Psoriatic Arthritis
There is no single specific test for psoriatic arthritis. A combination of factors will be assessed:
- Presence of psoriasis – Confirmed by a dermatologist.
- Pattern of joint involvement – Asymmetric arthritis in hands, feet and lower back.
- Blood tests – General markers of inflammation may be elevated.
- Physical exam – Check for nail changes, swollen joints, sausage toes.
- Imaging – X-rays, MRI or ultrasound to detect joint damage.
- Medical history – Your doctor will ask about symptoms and family history.
- Eye exam – To screen for uveitis (eye inflammation).
A rheumatologist and dermatologist will work together to reach a conclusive Psoriatic Arthritis diagnosis if joint symptoms are present.
Treating Psoriatic Arthritis
Psoriatic Arthritis treatment aims to relieve pain, reduce inflammation, slow joint damage and improve functioning. There is no cure at this time, so managing symptoms is key.
Common treatments for psoriatic arthritis include:
- NSAIDs – Anti-inflammatory medications like ibuprofen to relieve pain.
- Corticosteroids – Powerful steroids such as prednisone to quickly control flares.
- DMARDs – Disease-modifying antirheumatic drugs such as methotrexate.
- Biologics – Advanced medications like adalimumab that target specific cytokines.
- Light therapy – Phototherapy to help clear psoriasis skin symptoms.
- Alternative therapies – Fish oil, turmeric supplements, acupuncture or massage.
- Weight loss – Losing excess pounds reduces inflammation.
- Exercise – Gentle routines improve mobility and flexibility.
Early and aggressive treatment is key to prevent irreversible joint damage. Treatment is customized to the individual case by a rheumatologist.
Rheumatoid Arthritis vs. Psoriatic Arthritis: Key Differences
Now that we’ve covered the basics of rheumatoid arthritis and psoriatic arthritis separately, let’s summarize the main differences between Rheumatoid Arthritis and Psoriatic Arthritis:
- Presence of psoriasis – Psoriatic Arthritis only occurs in those with psoriasis. Rheumatoid Arthritis has no relation to skin disease.
- Seronegative factor – Blood tests for Psoriatic Arthritis antibodies are typically negative. Rheumatoid Arthritis tests are positive.
- Joint patterns – Rheumatoid Arthritis is symmetric and affects matching joint pairs. Psoriatic Arthritis is asymmetric.
- Spinal involvement – Psoriatic Arthritis frequently affects the lower spine. Rheumatoid Arthritis does not.
- Extra-articular symptoms – Psoriatic Arthritis can involve the eyes, skin and nails. Rheumatoid Arthritis primarily impacts joints.
- Gender ratio – Rheumatoid Arthritis is 3 times more common in women. Psoriatic Arthritis affects men and women equally.
- Age of onset – Rheumatoid Arthritis tends to begin in middle age between 30-60. Psoriatic Arthritis often starts earlier between ages 20-40.
- Joint damage – Rheumatoid Arthritis causes more erosion of bone. Psoriatic Arthritis has more new bone formation.
While they share some similarities, you can see there are distinct differences between rheumatoid and psoriatic arthritis.
Is My Joint Pain Caused by Rheumatoid Arthritis or Psoriatic Arthritis?
If you’ve been experiencing chronic joint pain, swelling and stiffness, it could potentially be rheumatoid arthritis or psoriatic arthritis. But how can you tell which one you might have?
Consider the following factors:
- Do you have psoriasis? If yes, you likely have psoriatic arthritis rather than rheumatoid arthritis.
- Are your joints symmetrically affected? Rheumatoid Arthritis usually impacts joints equally on both sides.
- Does pain/stiffness tend to affect your lower back, neck, fingers or toes? These are classic Psoriatic Arthritis hotspots.
- Do your blood tests show elevated inflammatory markers? That leans more towards Rheumatoid Arthritis.
- Does arthritis run in your family? A family history makes either Rheumatoid Arthritis or Psoriatic Arthritis more likely depending on the type.
- Are symptoms consistently worse in the mornings? This is very characteristic of Rheumatoid Arthritis.
Pay close attention to the pattern of your joint pain and which areas are affected. Share all the details with your doctor. Seeing a rheumatologist is key for getting an accurate differential diagnosis.
Don’t Try to Self-Diagnose – See a Rheumatology Specialist!
If you think your symptoms may be indicative of inflammatory arthritis, don’t try to self-diagnose. Getting an accurate diagnosis requires seeing the appropriate specialist – a board certified rheumatologist.
Rheumatologists complete many years of specialized training to diagnose and treat all forms of arthritis. They will perform a thorough evaluation including a physical exam, medical history, family history, diagnostic tests and imaging if needed.
This allows them to reach the correct specific diagnosis between conditions like rheumatoid arthritis, psoriatic arthritis, gout, lupus and various other types of arthritis.
Once diagnosed, the rheumatologist will create a tailored treatment plan to manage your symptoms and preserve joint health. Early treatment is crucial for the best outcomes.
Don’t delay – if you have chronic joint pain, fatigue and stiffness lasting over 6 weeks, make an appointment with a rheumatologist for proper evaluation.
Connecting With a Rheumatologist Has Never Been Easier
Traditionally, seeing a specialist like a rheumatologist has involved a referral process and long lag times for appointments. But with telemedicine, connecting with a rheumatologist is now quicker and more convenient than ever before.
Rheumatologist OnCall offers on-demand telehealth access to board certified rheumatology specialists. You can have a video consultation from the comfort of your own home – without needing to take time off work or school for an in-office visit.
Key benefits of Rheumatologist OnCall include:
- Fast access to rheumatology experts
- Convenient tele-visits by phone, tablet or computer
- Help determining if your symptoms require in-person evaluation
- Guidance choosing between rheumatoid arthritis vs. psoriatic arthritis diagnosis
- Prioritize your symptoms to create an optimal treatment plan
Don’t play guessing games with your joint pain. Get answers and a professional rheumatology opinion fast through Rheumatologist OnCall. Simply sign up online for same-day telehealth appointments.
Take Control of Your Joint Health
Arthritis symptoms like chronic joint pain and stiffness shouldn’t be ignored. Left untreated, rheumatoid arthritis and psoriatic arthritis can progressively damage joints and impair mobility over time.
Catching these conditions early is key to preserving joint function and quality of life. While Rheumatoid Arthritis and Psoriatic Arthritis share some similarities, there are important differences in their symptoms, causes and treatment approach.
If you notice persistent joint swelling and pain, make seeing a rheumatologist a priority. Getting an accurate diagnosis is the critical first step to halting inflammation and preventing permanent joint erosion down the road.
With convenient telemedicine options through Rheumatologist OnCall, getting answers about your joint pain and access to arthritis specialists is now quicker than ever. Don’t wait – take control of your joint health!