SHARE
There is always a delicate balance between the benefits and risks of taking a medication. Some patients are much more sensitive than others and are prone to side effects. In this article, I will discuss all you need to know about drug-induced lupus, from the most common medications to possible medications and the most likely clinical signs. I will discuss the types of antibodies seen and if drug-induced lupus is as severe as systemic erythematous lupus.
Let’s begin!
What is drug-induced lupus?
Drug-induced lupus is a lupus-like illness that occurs only in some people after exposure to a medication. Lupus is an autoimmune disease that can target many organs, from the skin to the heart, lungs, or kidneys. However, this is systemic erythematous lupus.
In the contrary, drug-induced lupus may be seen as a side effect of one medication. It may occur a few weeks after starting the medication up to one year later. It will appear more likely in elderly adults > more than 50 years in age in comparison with systemic lupus, which usually affects young adults.
What medications can cause drug-induced lupus?
Many medications are now known to cause drug-induced lupus, but here are the ten most common drugs that were frequently associated with this disease. Some of these medications are used for heart conditions, while others are used as anti-fungal or antibiotics.
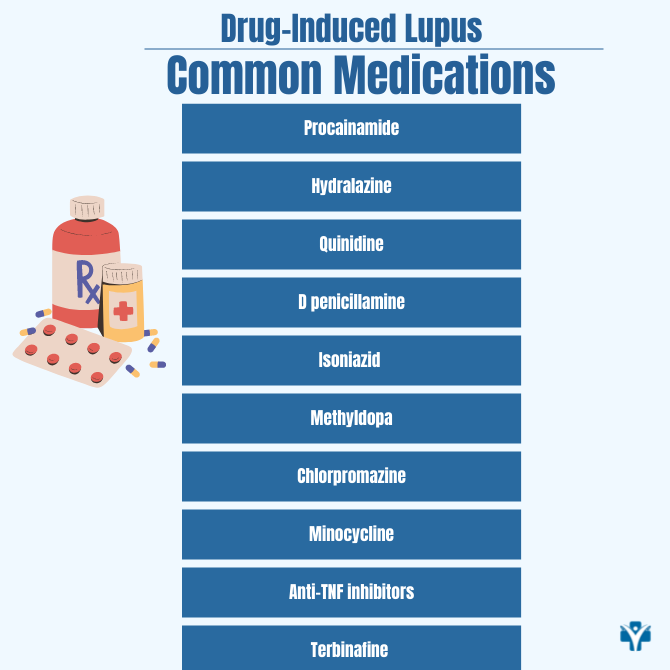
- Procainamide (used for heart arrhythmia)
- Hydralazine (used to decrease blood pressure)
- Quinidine (used for heart arrhythmias)
- D-penicillamine (used to treat Wilson’s disease)
- Isoniazid (used to treat tuberculosis)
- Methyldopa (used to reduce blood pressure)
- Chlorpromazine (used to treat mental disorders)
- Minocycline (used as an antibiotic)
- Anti-TNF inhibitors (used for inflammatory arthritis e.g. rheumatoid arthritis, psoriatic arthritis)
- Terbinafine (used as anti-fungal medication)
In 2019, I published the case of one of my patients. This was a 57-year-old Caucasian male with a past medical history of hypertension and hyperlipidemia presented with recurrent fevers, chest pain, and dyspnea. Initial evaluation revealed diffuse ST elevations, small pericardial effusion, anemia, and leukopenia. He was initially treated with non-steroidal anti-inflammatory drugs and prednisone for pericarditis. Six months later, he reported fatigue, arthralgia, morning stiffness, weight loss, fevers, and night sweats. Laboratory tests revealed persistent anemia and leukopenia. Extensive workup, including bone marrow biopsy and infectious evaluations, was negative. Autoimmune workup, however, revealed positive anti-histone and anti-chromatin antibodies despite negative antinuclear antibody. A diagnosis of drug-induced lupus secondary to hydrochlorothiazide was made. The medication was stopped, and prednisone was initiated, resulting in marked improvement in his symptoms and hematologic abnormalities.
Many other drugs can cause drug-induced lupus, here I will include an more extended list:
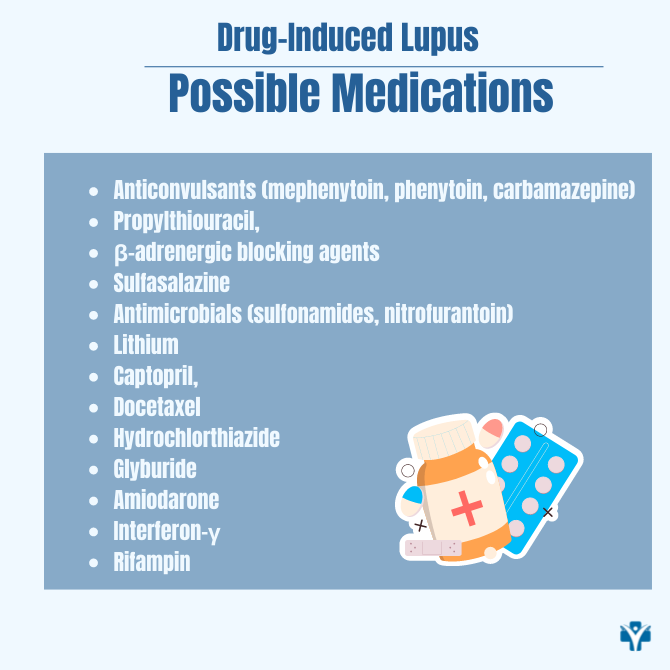
- Anticonvulsants (mephenytoin, phenytoin, carbamazepine)
- Propylthiouracil
- β-adrenergic blocking agents
- Sulfasalazine
- Antimicrobials (sulfonamides, nitrofurantoin)
- Lithium
- Captopril
- Docetaxel
- Hydrochlorthiazide
- Glyburide
- Amiodarone
- Interferon-γ
- Rifampin
What are the most common clinical signs?
The way patients with Drug-induced lupus present to my rheumatology consultation can vary greatly. However, most patients will describe unspecific symptoms such as fevers, night sweats, and unintentional weight loss. Some patients will describe joint pain involving multiple small or big joints. Muscle pain that is diffuse and bothersome can also be present. More rarely, patients present with complaints of chest pain or pain when they take a deep breath.
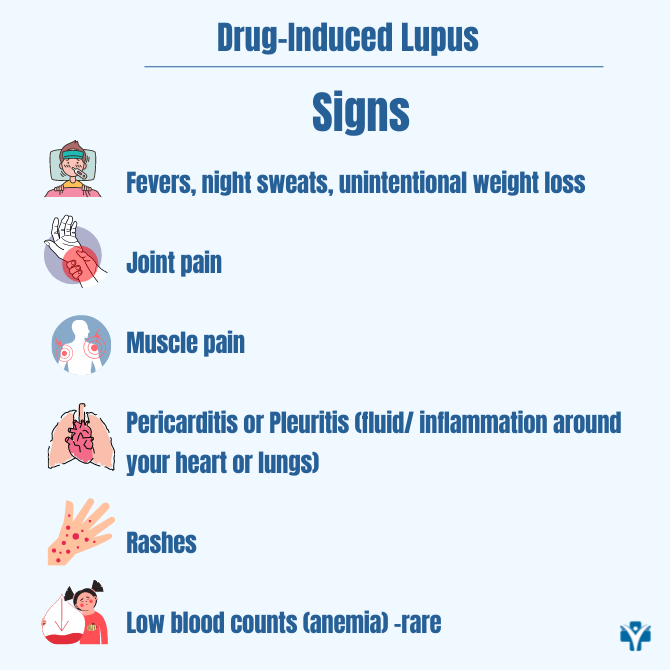
At times, they have to limit breathing due to chest pain. Some patients are diagnosed with fluid/ inflammation around the heart or lungs called “pericarditis or pleuritis”. Other patients present with rashes on their face, chest, or back that can come and go or be persistent. Very rarely, based on the blood work, patients can present with a decrease in the cell counts (low white blood cells, anemia, low platelet count). Kidney function is usually normal, but I always check the patient’s renal function, as kidney dysfunction is rarely seen.
What are auto-antibodies commonly seen in Drug-induced lupus?
In rheumatology, we order many laboratory tests. When we suspect lupus or a lupus-like reaction, we order specific laboratory workup. It is essential to distinguish between systemic lupus and drug-induced lupus clearly.
The most common antibodies I see in patients with Drug-induced lupus are positive antinuclear antibodies (positive ANA test). If you want to learn more about what a positive ANA means, read my blog or watch this video in my Youtube channel.
However, a positive ANA test does not make the diagnosis of lupus. For example, a drug (e.g, procainamide) can cause a positive ANA test but will not necessarily cause Drug-induced lupus. Only 30% of patients that used procainamide and had a positive ANA test also developed Drug-induced lupus.
The second common type of autoantibodies seen in drug-induced lupus are the anti-histone antibodies. However, these are not specific to Drug-induced lupus and can be seen even in patients with systemic erythematous lupus. The presence of anti-histone antibodies can lead to a drug-induced reaction.
The confusion comes when we find another type of antibody called “double stranded-DNA antibodies“. These types of autoantibodies are more specific to systemic erythematous lupus, but they may be rarely found in patients that developed Drug-induced lupus after exposure to TNF- alpha inhibitors (e.g. remicade/ infliximab; humira/ adalimumab or Enbrel/ etanercept etc).
Is Drug-induced lupus as severe as systemic lupus?
Drug-induced lupus tends to be a more limited disease when compared to systemic lupus. In most patients, drug induced lupus can affect the skin, joints, and muscles and can give patients fevers, but it tends not to involve significant organs. In comparison, systemic lupus is more aggressive disease and it tends to affect major organs like the brain, heart, lungs, and kidneys. You will always need a thorough evaluation to make sure the drug induced lupus is not involving major organs.
To make the correct diagnosis of Drug-induced lupus, you need the help of an experienced rheumatologist that will be able to correlate your signs, symptoms, and laboratory workup. This is an educational article that aims to broaden your knowledge, but it does not offer you medical advice. If you have an autoimmune disease and you need help, you are welcome to check out our practice and get the help that you need when you need it the most. Rheumatologist OnCall is a telemedicine rheumatology practice that broadens access to a specialist in a very short time, when you need it the most, and breaks geographical barriers. Check out the states where we are licensed to see patients in the US and reach out to us if needed. We are happy to serve you.














